Your prescription drug plan through Express Scripts offers low co-pays for generic medication, a convenient way to get 90-day prescriptions filled, and a specialty pharmacy for some long term health conditions that require special medicines.
Your Prescription and Pharmacy Coverage
Prescribed a high cost specialty medication?
If so, contact Accredo Specialty Pharmacy.
Use this card when you go to the dentist
(The Member ID starts with a "U" - this IS NOT your UBC Number)
Prescription & Pharmacy Coverage FAQs
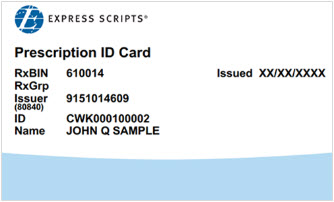
Prescriptions are paid by using your Express Scripts card.
No. You can fill a 90 day supply at either Express Scripts Mail Order or by using a CVS Pharmacy. Please note, if you fill a medication more than 3 times, you will have to fill the 4th fill at one of these options. If you use a Pharmacy other than Express Scripts or CVS, you will pay 100% of the cost of the medication.
Non-Preferred Brand Medications typically offer a generic substitute to safely and effectively treat medical conditions. If you are prescribed a Non-Preferred Brand Medication, you will be responsible for 40% of the total cost of the medication. By asking for generic substitutes wherever possible, you maximize your savings. Only you and your prescribing Physician can determine if a generic substitute is right for you. If you're unable to take a generic substitute for your Non-Preferred Medication, ask your Prescribing Physician for samples, or manufacturer's coupons when possible.
Preferred Brand Medications ordinarily do not offer a generic substitute. For Preferred Brand Medications, you will never pay more than $75.00 out-of-pocket for a 30-day supply, or $150.00 for a 90-day supply. Click the following link for the Express Scripts Preferred Drug List to see if your Medication is considered a Preferred Brand. You may also visit Express Scripts online at www.express-scripts.com for a comprehensive list.
You can call the Fund Office at 732-417-3900 and we will request a new Express Scripts card for you, or call Express Scripts at 1-800-939-2146 or visit their website at www.express-scripts.com
Yes, for Plan Year April 1, 2022 through March 31, 2023, the prescription out-of-pocket maximum is:
- $6,000 Individual, or
- $12,000 Family
Once an individual or family has reached their OOP Max, the Fund will pay 100% for all further eligible claims for the duration of the Plan Year.



